What is glaucoma?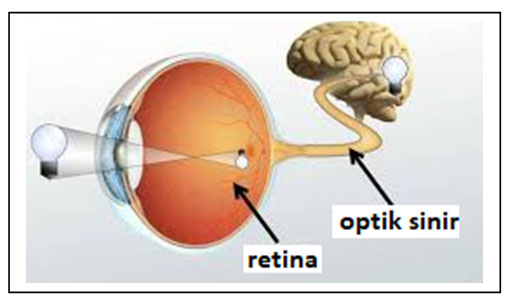
Glaucoma; The thin nerve layer that surrounds the inner surface of the eye like a sheet and creates visual signals is called the retina.
Visual signals generated by photoreceptors (vision cells) in the retina are carried to the visual center in the brain by thin nerve cells called axons. All the axons come together at a place called the optic nerve head and form the optic nerve.
The optic nerve is made up of about 1 million nerve fibers. We can compare the optic nerve to an electrical cable containing hundreds of thousands of thin wires.
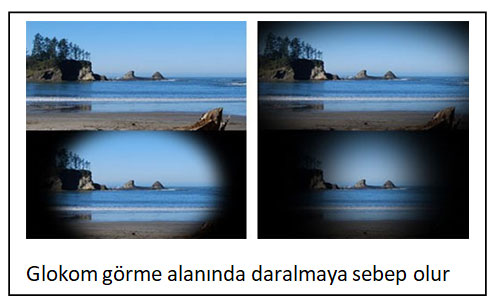
Glaucoma is a disease that causes progressive damage to the optic nerve and loss of vision. Loss of each nerve fiber also causes a loss in the visual field.
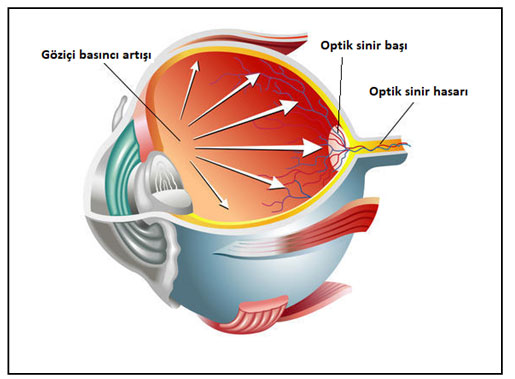
It is also known as eye pressure, as the damage in glaucoma is usually due to an increase in intraocular pressure.
The expression of eye pressure can be misleading, as a quarter of patients can also suffer damage without increasing their eye pressure, or because some people with high eye pressure do not develop glaucoma. Glaucoma is the second most common cause of blindness in the world.
What is the relationship between intraocular pressure and glaucoma?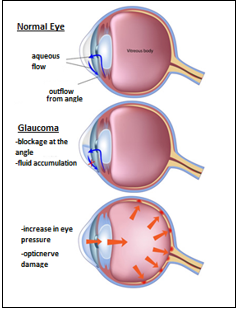
The eye fluid that fills the eye and nourishes the intraocular structures is called aqueous. While the intraocular fluid is continuously produced and it is continuously absorbed and discharged out of the eye.
The structure where the fluid is produced is called the ciliary body, and the place where it is absorbed is called the anterior chamber angle. The place where the fluid is absorbed at the anterior chamber angle is similar to a filter or strainer.
If the fluid is produced in excess or there is a problem in its absorption, the intraocular pressure increases. The increase in intraocular pressure is mostly due to a problem in absorption.
When the intraocular pressure increases, pressure on the optic nerve head occurs and damage to the optic nerve occurs. If it is left untreated, the damage is permanent and causes blindness.
What are the types of glaucoma?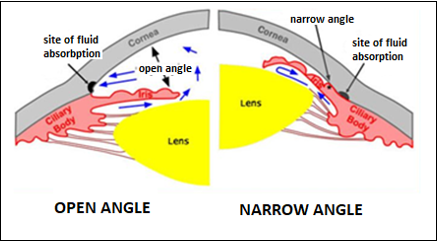
Glaucoma is anatomically divided into two types as open-angle or angle-closure (narrow-angle).
In open-angle glaucoma, the angle anatomy, where the eye fluid is absorbed, is normal, and the occlusion is in the micro-channels at the angle.
On the other hand, in angle-closure glaucoma, the angle is covered by the iris, which is the colored part of the eye, and fluid absorption is therefore reduced.
Glaucoma is also classified as primary glaucoma or secondary glaucoma based on its root cause. In primary glaucoma, intraocular pressure increases for no apparent reason. Secondary glaucoma occurs due to reasons such as another disease, drug use, trauma and eye surgery.
Although there are nearly 50 types of secondary glaucoma, they are very rare. The most common glaucoma is primary open angle glaucoma.
Primary Open Angle Glaucoma: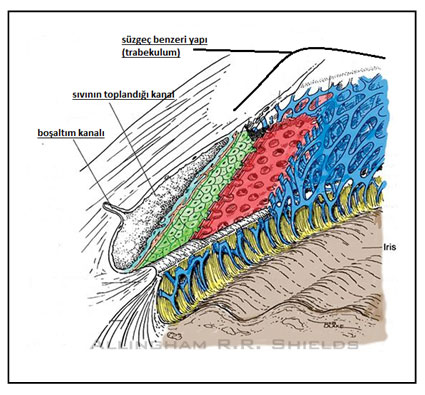
About 90% of glaucoma patients have primary open-angle glaucoma. In this disease, although the anterior chamber angle is open, there is a blockage in the filter-like structure through which the fluid is absorbed.
There is no specific reason for the blockage. As a result, fluid absorption is impaired and intraocular pressure increases.
In this type of glaucoma, there is no pain and the vision level is not affected in the early period. In other words, the patient may not realize that there is a problem until the disease progresses. However, it can be detected during routine examination.
Some people’s optic nerve is very sensitive to increased intraocular pressure. In other words, even if the increase in pressure remains within normal limits, damage to the optic nerve occurs. This type of open-angle glaucoma is called normal-tension glaucoma.
Narrow Angle Glaucoma (or angle closure glaucoma):
In this type of glaucoma, the iris, the colored part of the eye, covers the angle where the fluid is absorbed and makes absorption difficult. If it does not completely cover the angle, a clinical picture similar to primary open-angle glaucoma occurs. In other words, optic nerve damage develops insidiously and slowly and the patient does not realize that there is a problem. This is called chronic angle-closure glaucoma.
Sometimes, the iris completely covers the angle and the intraocular pressure increases suddenly, causing complaints such as severe pain, nausea-vomiting, colored wavy vision and vision loss. This condition is called an acute angle-closure attack. If it is not intervened immediately when an attack occurs, it can quickly cause blindness.
What is the suspicion of ocular hypertension and glaucoma?
Ocular hypertension is a condition in which the intraocular pressure is measured above the normal limit and no optic nerve damage is detected in the tests. These patients are considered to have a suspicion of glaucoma. In some patients, a suspicious finding in the examination or a suspicious disorder in the tests may be detected but the intraocular pressure may be low. These patients are also considered to have a suspicion of glaucoma. Patients with a suspicion of glaucoma are considered to be at high risk of developing glaucoma in the coming years. Close follow-up of these patients by an ophthalmologist is important for early detection of glaucoma and timely initiation of treatment.
Who are at risk of glaucoma and what should they do?
High intraocular pressure (10-21 mm Hg is normal) is the most important risk factor for glaucoma. Additionally, glaucoma-related optic nerve damage may develop in approximately one quarter of patients even without increased intraocular pressure.
This condition is called normal-tension glaucoma and the role of vascular factors has been demonstrated. Therefore, those with vascular diseases such as hypertension and hypotension, ischemic brain and heart disease, atherosclerosis, migraine and Raynaud’s disease are considered to be at increased risk of glaucoma.
Genetic factors also have an important place among the risk factors, people with a family history of glaucoma (people with close blood ties) have a higher than normal risk of glaucoma. High myopia and corneal thickness below 520 microns also increase the risk of glaucoma.
What are the symptoms of glaucoma and what complaints does it cause?
Glaucoma is an insidious disease. The patient usually does not realize the condition because it does not show any symptoms in the early stages. It is difficult to detect by measuring intraocular pressure only, even in routine eye examination.
The reason for this is that the intraocular pressure changes during the day and it is possible to measure the pressure as normal during the measurement in the examination.
For this reason, it has been determined in studies that there is an undiagnosed patient group as much as the number of diagnosed glaucoma patients. When the disease progresses, the visual field gradually narrows and the patient begins to have difficulty seeing the sides.
If the intraocular pressure increases suddenly and too much (acute angle closure attack), it causes complaints such as pain, blurred vision, nausea-vomiting, otherwise it does not give any symptoms. When glaucoma causes decreased vision, we are now in the final stage.
How is glaucoma diagnosed?
Glaucoma causes progressive damage to the optic nerve and loss of the visual field. In the diagnosis and follow-up of glaucoma, tests evaluating the optic nerve and visual field should also be performed together with the measurement of intraocular pressure. Measuring intraocular blood pressure only is not sufficient to diagnose glaucoma and determine the damage that has occurred.
- Intraocular pressure measurement (tonometry): Intraocular pressure measurement is done regularly for both diagnosis and follow-up of glaucoma. This measurement can be made in one of several ways. A practical instrument is generally used to measure intraocular pressure by blowing air into the eye (air-puff) in the outpatient clinic. The applanation tonometer, on the other hand, measures the intraocular pressure according to the flattening of the cornea by contacting the eye. Since it gives more accurate results than the air-puff method, it is preferred more in the diagnosis and follow-up of glaucoma. Although there is no definite rule, the normal range of intraocular pressure is between 10-20 mmHg.
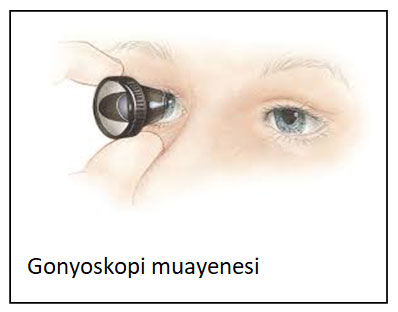 Eye angle examination (gonioscopy): In this examination, a special lens is attached to the surface of the eye and the angle of the anterior chamber, where the intraocular fluid is absorbed, is examined. According to the examination results, the type of glaucoma (open-angle or angle-closure), trauma-related damage, adhesions etc. are determined. The treatment method to be chosen is determined according to these examination findings
Eye angle examination (gonioscopy): In this examination, a special lens is attached to the surface of the eye and the angle of the anterior chamber, where the intraocular fluid is absorbed, is examined. According to the examination results, the type of glaucoma (open-angle or angle-closure), trauma-related damage, adhesions etc. are determined. The treatment method to be chosen is determined according to these examination findings
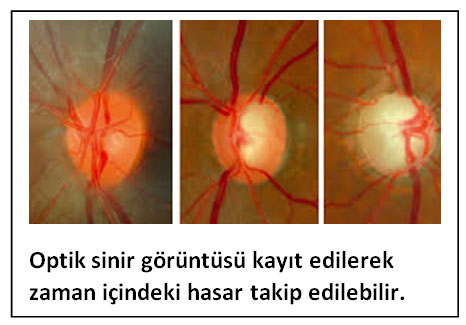 Optic nerve examination: The basic for performing optic nerve examination and detecting changes in optic nerve is fundoscopy with drop. After the routine eye examination, the pupils are dilated with drops and optic nerve at the back of the eye is examined with special lenses. Although the changes in the optic nerve can be seen easily with this method, they need to be monitored and recorded with special devices. Thus, your doctor can easily compare the changes in the optic nerve at later controls.
Optic nerve examination: The basic for performing optic nerve examination and detecting changes in optic nerve is fundoscopy with drop. After the routine eye examination, the pupils are dilated with drops and optic nerve at the back of the eye is examined with special lenses. Although the changes in the optic nerve can be seen easily with this method, they need to be monitored and recorded with special devices. Thus, your doctor can easily compare the changes in the optic nerve at later controls.- Corneal thickness measurement (pachymetry):Corneal thickness measurement should be taken in all patients with suspected or diagnosed glaucoma. Because corneal thickness directly affects the result of eye pressure measurement. Intraocular pressure is measured higher than normal in people with thicker than normal corneas, and lower than normal in people with thinner than normal corneas. For example, although the intraocular pressure of a person with a thick cornea is measured high, it may actually be within normal limits. In other words, the risk of developing glaucoma is lower than a person with a thin cornea. Since corneal thickness varies from person to person, measurement should be taken once from all patients.
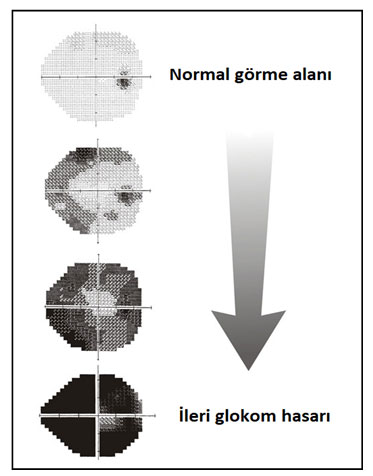 Visual field test (perimetry):Even if the patient’s intraocular pressure is normal in the follow-up examinations, if there is a progressive loss in the visual field, the treatment is considered to be insufficient.In glaucoma patients, progressive damage to the optic nerve and consequent narrowing of the visual field occurs. The visual field test is a test that evaluates the function of the optic nerve. Visual field measurement is important both in the diagnosis and in the follow-up of the disease. If the loss in the visual field does not progress, the disease is under control.
Visual field test (perimetry):Even if the patient’s intraocular pressure is normal in the follow-up examinations, if there is a progressive loss in the visual field, the treatment is considered to be insufficient.In glaucoma patients, progressive damage to the optic nerve and consequent narrowing of the visual field occurs. The visual field test is a test that evaluates the function of the optic nerve. Visual field measurement is important both in the diagnosis and in the follow-up of the disease. If the loss in the visual field does not progress, the disease is under control.- Retinal nerve fiber thickness measurement: Damage to the optic nerve can be detected by measuring retinal nerve fiber thickness. This measurement is made with a device called optical coherence tomography (OCT). Gradual decrease in nerve fiber thickness is an indication of the progression of glaucoma damage.
How is glaucoma treated?
Since the damage in glaucoma cannot be reversed, the main purpose of treatment is to prevent the progression of the damage to the optic nerve.
Since the most important risk factor for the development of damage to the optic nerve is intraocular pressure, almost all treatment methods are aimed at lowering intraocular pressure.
Lowering intraocular pressure can prevent or at least slow the damage in many patients. There are many treatment methods in glaucoma, and the patient and ophthalmologist should decide together which treatment to apply.
- Medical (drug-drop) treatment: Glaucoma is a disease that can usually be controlled with eye drops. Glaucoma medications help to reduce intraocular pressure and prevent visual field loss. It is necessary to use these drugs on a very regular basis every day. In cases where a single drug is not enough, more than one drop can be used. Like any medication, glaucoma medications have side effects. These may include eye-specific side effects such as redness, burning, stinging, and change in skin color around the eyes, as well as general side effects such as fatigue, weakness, shortness of breath, and palpitation. You should definitely inform your doctor when side effects develop. Your doctor may change the medication depending on the situation.
- Laser surgery:
- Laser trabeculoplasty: It is used in the treatment of open angle glaucoma. It is aimed to increase the fluid absorption by applying a laser beam to the anterior chamber angle where the fluid is absorbed. This procedure is performed on an outpatient basis under outpatient conditions. Its effectiveness is usually 2-3 years.
- Laser iridotomy: It is used for the prevention or treatment of acute angle closure attack in angle-closure glaucoma. Fluid flow is facilitated by making a hole in the iris, which is the colored part of the eye.
- Laser cyclophotocoagulation: The ciliary body, where the intraocular fluid is produced, is destroyed by laser and the production of intraocular fluid is reduced. It is generally applied in refractory glaucoma patients who do not respond to other treatment.
- Glaucoma surgery:
- Trabeculectomy: It is the most commonly used method and the gold standard in glaucoma surgery today. It is successfully applied in glaucoma patients who cannot be treated with drugs. In this surgery, a part of the anterior chamber angle where the fluid is absorbed is removed and fluid drainage is provided through a new channel. Thus, a continuous and balanced decrease in intraocular pressure is achieved.
- Glaucoma valve surgeries: In some risky intraocular pressure types or in eyes that have not been successful with trabeculectomy, drainage of intraocular fluid is provided with the help of artificial tubes. It is generally preferred in difficult cases and special situations.