What is Diabetic Retinopathy?
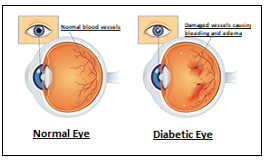
Diabetic Retinopathy; The thin nerve layer that surrounds the inner surface of the eye like a sheet and creates visual signals is called the retina. The retina is nourished by a large number of thin retinal vessels.
High blood sugar in diabetes damages the retinal vessels over time. As a result, the nutrition of the retina is disturbed, bleeding and edema (fluid accumulation) occur.
The retina cannot fulfill its function, so vision loss occurs. If not treated on time, irreversible vision loss, ie blindness, may occur. Diabetic retinopathy is one of the leading causes of blindness.
As in the whole world, the incidence of diabetes and diabetic retinopathy is increasing in Turkey and continues to be a serious public health problem.
What are the risk factors for diabetic retinopathy?
Anyone with diabetes is at risk for the development of diabetic retinopathy. In the studies conducted, the duration of diabetes was determined as the most important risk factor for the development of diabetic retinopathy.
The longer the duration of diabetes, the greater the risk of developing diabetic retinopathy. Diabetic retinopathy is present in 50% of 10-year diabetes patients and 90% of 30-year patients. Keeping blood glucose value in balance can be considered as the second most important factor.
The longer the blood sugar is kept in balance, the later and the milder the development of diabetes. Apart from these, conditions such as hypertension, high cholesterol level and pregnancy increase the risk and severity of developing diabetic retinopathy.
The type of diabetes may also be a determinant for retinopathy. In type 1 diabetes patients, retinopathy may develop at an earlier age and more severely.
Are there types of diabetic retinopathy?
There are two types of diabetic retinopathy.
- Non-proliferative Diabetic Retinopathy: There is no new vessel formation in this type. If there is edema in the macula and it causes decreased vision, treatment is required. If there is no edema in the macula, it is followed.
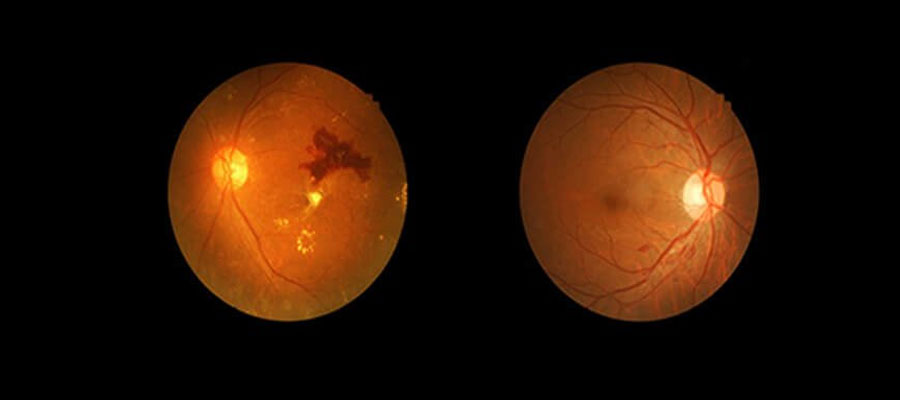
- Proliferative Diabetic Retinopathy: It is characterized by the formation of new vessels. Laser treatment must be applied, otherwise it may cause blindness by bleeding into the eye. If there is edema, the edema is treated first and then laser is applied.
How does diabetes damage the retina?
The main cause of diabetic retinopathy is the rise in blood glucose, which damages the retinal vessels and sometimes causes these vessels to become blocked.
When the vessels in the visual center (macula) are damaged, the fluid in the vessel leaks into the retina and causes the retina to swell like a sponge.
This adversely affects the vision cells and a decrease in vision occurs. If edema is not treated, the damage to the cells becomes permanent.
Over the years, the damage spreads to the retina and abnormal veins and membrane formations develop on the retinal surface.
If it is left untreated, new vein formations cause serious intraocular hemorrhages and the membranes shrink and pull the retina away from where it is attached. Over time, new vein formations may envelop the entire eye, leading to severe eye pressure and blindness.
What are the symptoms of diabetic retinopathy?
Diabetic retinopathy is an insidious disease. It can progress for years without symptoms. By the time symptoms appear, the disease may be very advanced. Therefore, every diabetic patient should go through a routine eye examination annually.
Symptoms may be in one or both eyes. These are:
- blurred vision
- diplopia
- difficulty in distinguishing colors
- difficulty in reading
- floaters and shadows
- feeling of pressure and pain in the eye.
How is diabetic retinopathy diagnosed?
The basic method in the diagnosis of diabetic retinopathy is fundus eye examination with eye drops. After the routine eye examination, the pupils are dilated with drops and the back of the eye (retina) is examined with special lenses.
In this examination, fluid accumulation (edema), bleeding, impaired vascular structures and new vessel formations are sought. According to the examination findings, your doctor may request eye angiography and/or eye tomography (OCT-optical coherence tomography) examinations.
These tests determine the stage of the disease. Additionally, it is decided whether treatment is required, what treatments to do if required, and how often to follow-up.
What treatment options are available for diabetic retinopathy?
No matter what treatment is applied in diabetic retinopathy, the most important factor affecting the success of the treatment in the long term is keeping blood glucose under control strictly.
Keeping blood glucose under strict control will both increase the success of the treatment and prolong its effectiveness. Hemoglobin A1C (3-month glucose) levels are checked at regular intervals and the general course of blood glucose is followed.
Additionally, if the patient has hypertension, treatment must be provided. Otherwise, it will be difficult to get the desired response from the treatment of retinopathy. It should not be forgotten that the best treatment is prevention.
There are several methods of treating retinopathy. These are:
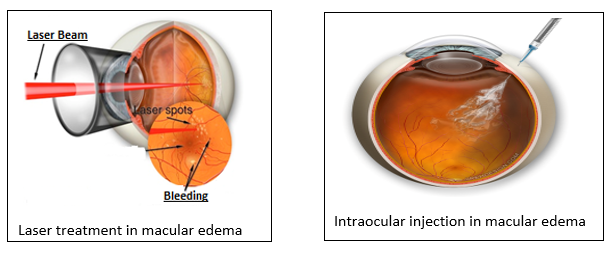
1) Laser Treatment: Laser treatment can be applied in regional (small) macular edema that does not involve the entire macula and its center. According to the results of eye angiography and eye tomography, small burns are made to the fluid leaking areas with laser beams and the edema is healed. It may take several months for the edema to regress.
The laser is also used in the treatment of new vessel formations. Laser burns are applied to retinal areas with impaired blood supply in a few sessions. Thus, new vessel formations are destroyed. Intraocular bleeding, that is, the risk of surgery and blindness, is prevented.
2) Intraocular injections: It is the most common treatment for vision reduction due to macular edema (fluid accumulation in the visual center). The drugs given intraocularly prevent the vessels from leaking and the edema heals.
Usually, more than one injection is required at regular intervals. There are several different types of drugs available today. The drug to be applied is determined by the condition of the eye and the preference of the physician.
3) Vitrectomy surgery: If treatment is delayed or blood glucose cannot be kept under tightly control, the disease may progress despite everything. This causes intraocular hemorrhage and the formation of shrinking membranes in the retina.
If this stage has been reached, there is no other option but surgery. Vitrectomy surgery is required. In vitrectomy surgery, very small holes are made in the eye and the eye is entered. Eye bleeding and membranes on the retinal surface are cleaned.
Laser is applied to retinal areas with impaired blood supply. The results of surgery are depending on timing. Today, thanks to the development of surgical techniques, satisfactory results are obtained in cases with early intervention.